Most people with tuberous sclerosis complex (TSC) have changes in their skin. Nearly all people with TSC develop at least one skin feature during their lifetime, and many will have several. Some TSC skin features may appear at birth, while others may appear later in childhood or even in adulthood.
Currently, there is no way to predict how many TSC skin features will develop in an individual.
The occurrence of specific types of skin features of TSC is highly variable from one individual with TSC to the next, even within one family. Some people have TSC skin changes that are hardly noticeable. Others may have growths on the skin that cause pain or bleed easily. In addition, changes on the skin often occur in cosmetically important areas of the body such as the face.
A variety of specific types of skin changes or lesions, described below, can occur in a person with TSC. When occurring in certain combinations in a single person, they can be used to make a definitive TSC diagnosis.
Facial angiofibromas
 Facial angiofibromas are tumors on the face that often appear across the checks and nose and on the chin. They are initially small spots or bumps that may increase in size with age. Angiofibroams in light-skinned people may be skin-colored, pink, or red due to increased blood flow in these lesions. In darkly pigmented individuals they may be reddish brown or dark brown. Facial angiofibromas are rarely present at birth, but often begin to appear anytime from early childhood to early adulthood. Most individuals with TSC will develop facial angiofibromas, but some will not. The major problems associated with angiofibromas are that they can become painful, may cause recurrent bleeding concerns or, rarely, nasal airway obstruction. Also, visible facial lesions, depending on the individual and severity of lesions, may lead to challenges in social situations at any age, but especially in school-aged children and young adults.
Facial angiofibromas are tumors on the face that often appear across the checks and nose and on the chin. They are initially small spots or bumps that may increase in size with age. Angiofibroams in light-skinned people may be skin-colored, pink, or red due to increased blood flow in these lesions. In darkly pigmented individuals they may be reddish brown or dark brown. Facial angiofibromas are rarely present at birth, but often begin to appear anytime from early childhood to early adulthood. Most individuals with TSC will develop facial angiofibromas, but some will not. The major problems associated with angiofibromas are that they can become painful, may cause recurrent bleeding concerns or, rarely, nasal airway obstruction. Also, visible facial lesions, depending on the individual and severity of lesions, may lead to challenges in social situations at any age, but especially in school-aged children and young adults.
Hypomelanotic macules
Hypomelanotic macules are flat areas of skin that appear lighter than the surrounding skin. They may informally be referred to as ash-leaf spots, because some are oval at one end and pointed at the other. They are not harmful or painful, so they are generally not treated. However, because they are often present at birth or soon thereafter, hypomelanotic macules are an important tool for diagnosing TSC. Hypopigmented macules are often more easily visualized under UV-light using a Wood’s lamp. “Confetti” skin lesions are areas of skin containing many very small hypopigmented spots.
Shagreen patch
The shagreen patch is a patch of skin similar in color to surrounding skin but tough and dimpled like an orange peel. The shagreen patch is usually found on the lower back and nape of the neck, but it may also be seen on other parts of the body.

Ungual fibromas
Ungual fibromas are small fibrous growths that appear around the fingernails or toenails and usually do not occur until adulthood. Ungual fibromas may require treatment because they can distort the nail by causing a groove or by pushing the nail up from the nail bed, which may lead to pain, infection or bleeding.
Fibrous cephalic plaque
Fibrous cephalic plaque may appear on the forehead or scalp of a person with TSC, and less commonly on the face. These plaques are usually compressible or doughy lesions.

Protection of skin from the ultraviolet (UV) light in sunlight is very important for individuals with TSC. Genetic studies have found evidence of UV-light-induced mutations in TSC1 or TSC2 genes in facial angiofibromas. This suggests that exposure of the face to sunlight could, over time, increase the development of facial angiofibromas. Also, hypopigmented macules are more susceptible to sunburn than normally pigmented skin. Sun protection may be achieved by applying sunscreen or by wearing a hat and clothing that covers the arms and legs.
First-line treatment of facial angiofibromas is generally topical mTOR inhibitor treatment. In 2022, the FDA approved the first topical rapamycin gel in the US for treatment of facial angiofibromas associated with TSC. For individuals in whom topical rapamycin is not effective or not an acceptable option, other treatments are available. In people with long-term facial angiofibromas, lesions may contain so much fibrous material that they will not shrink with mTOR inhibitor therapy. Examples of other options include ablative laser, surgical excision, dermabrasion, or cryosurgery. Removal is quick using these methods, but the scarring and changes in pigmentation that may result are permanent.
Ungual fibromas that become problematic or bothersome can be surgically removed by a dermatologist. Ungual fibromas may recur.
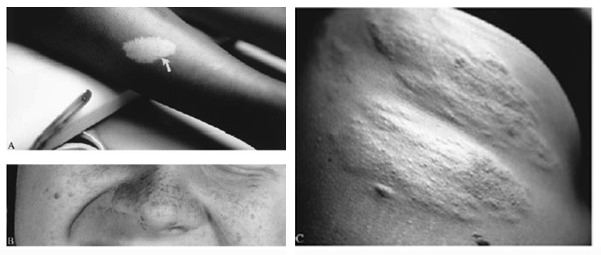
Figure 1. Classic cutaneous manifestations of tuberous sclerosis include (A) hypomelanotic macule (ash-leaf spot) (arrows), (B) facial angiofibromas. (C) Shagreen patch. Figures 1A and 1C reprinted from Roach ES, Semin Neurol 1988: 8:83-96, with permission. Figure 1B reprinted from Roach ES, Delgado MR, Derm Clin 1995;13:151-161, with permission.